Menstrual Cycle and Blood Sugar Levels: Does the Menstrual Cycle Affect Glucose Levels?
Understanding the Relationship Between Menstrual Cycle and Blood Sugar

Understanding the Relationship Between Menstrual Cycle and Blood Sugar
This article was last updated on November 2023
The menstrual cycle is a complex biological process that involves the cyclical maturation and release of an egg, controlled by a delicate interplay of hormones. While the hormonal changes during the menstrual cycle are primarily associated with reproductive function, they can also have significant effects on metabolism.
One such effect is on blood sugar levels and insulin resistance, which can vary across the menstrual cycle. Understanding these variations is important, as they may have implications for the management of conditions such as diabetes and polycystic ovary syndrome (PCOS) in women.
In this article, we will explore the relationship between the menstrual cycle, blood sugar levels, and insulin resistance, and discuss the potential implications for women's health.
What is the menstrual cycle?
The menstrual cycle is the process of ovulation and menstruation, which occurs on average every 28 days in most women. The cycle is regulated by a complex interplay of hormones, including estrogen and progesterone.
These hormones are responsible for preparing the uterus for pregnancy, as well as causing changes in the ovaries and other organs.
The menstrual cycle consists of two main phases: the follicular phase (approx days 1-14) and the luteal phase (approx days 15-28). Understanding the different phases of the menstrual cycle is essential in understanding the relationship between the menstrual cycle and glucose levels.
You can learn more about it in our in-depth article about The Menstrual Cycle – Phases, hormones, and their functions

How does the menstrual cycle affect blood sugar levels?
Historically, studies on how blood sugar levels change during the menstrual cycle have had mixed results. Some research shows that blood sugar changes with the cycle, especially during the luteal phase (after ovulation), while others found no significant changes. However, its important to note that these studies have had issues like small numbers of blood sugar tests, reliance on self-reported dates for menstruation, and not accounting for differences in body weight or physical activity, which could explain why the results vary from one study to another.
A more recent study conducted in August 2023, has shown that:
- Blood sugar was lowest during the late-follicular phase (just before ovulation), increased during ovulation, peaked in the luteal phase (after ovulation before menstruation), and then dropped sharply during menstruation.

- Higher estrogen levels were linked to lower blood sugar levels
- More physical activity (steps taken) was linked to lower blood sugar levels
- Food cravings tended to be associated with higher blood sugar levels, especially if the cravings were strong
- Some evidence suggested that feeling very tired might relate to lower blood sugar levels
- Sleep problems sometimes corresponded with higher blood sugar levels, though this wasn't always significant
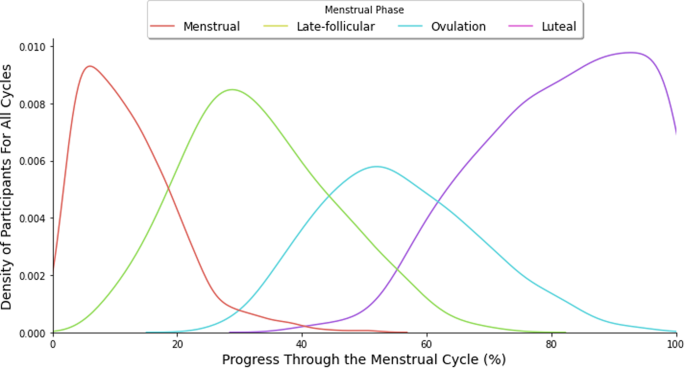
They found that sugar levels were highest during the Luteal phase (after ovulation, before menstruation) and lowest during the Late Follicular phase (just before Ovulation). These changes were consistent even when considering other factors like physical activity, estrogen levels, food cravings, tiredness, and sleep problems.

The study's findings support the idea that hormones like estrogen, which vary during the menstrual cycle, can affect metabolism and blood sugar levels. For instance, estrogen can reduce appetite and food cravings, which might help explain why blood sugar levels and food cravings vary during the cycle.
The study also suggests that daily blood sugar levels could be used to estimate different phases of the menstrual cycle. This could help people, particularly those with conditions like diabetes, to adjust their diets, sleep, or insulin therapy based on their menstrual cycle. However, it’s worth noting that women with diabetes may experience more significant changes in blood sugar levels during the menstrual cycle than women without diabetes.
Is blood sugar higher during your period?
As mentioned before, different stages of the menstrual cycle can have different effects on your blood sugar levels. Blood sugar levels are at their highest during the Luteal phase and start to descend during menstruation, reaching their lowest point in the Late Follicular phase. As you approach the luteal phase, these blood sugar levels naturally increase even further and you may experience some insulin resistance. Several studies ( have shown that a high concentration of progesterone is related to abnormal glucose metabolism, a high level of plasma glucose, and increased insulin resistance.
- Study 1: The effect of progesterone and pregnenolone on diabetes status in Chinese rural population: a dose–response analysis from Henan Rural Cohort
- Study 2: Blood Glucose Levels at Two Different Phases of Menstrual Cycle: A Study on a Group of Bengali-speaking Hindu Ethnic Populations of West Bengal, India
Hormonal Changes and Blood Sugar
As we already know, the menstrual cycle is a huge combination of changing hormones. We mentioned in the previous section, how blood sugar levels change in the menstrual cycle. Now let us dig a little further into the hormones responsible for blood sugar levels.
Which hormone increases blood sugar?
The hormone that is responsible for increasing your blood sugar is glucagon. Glucagon comes from alpha cells found in the pancreas, their primary function is to work with other hormones and bodily functions to control glucose levels in the blood. In simple terms, they increase blood sugar levels when they go too low.
Which hormone decreases blood sugar?
The hormone that is responsible for decreasing your blood sugar is insulin. A cell's ability to absorb glucose is mediated by insulin, which allows the muscle, fat, and liver to absorb glucose from the blood. Glucose can serve as energy or be converted into fat as needed.
Can high insulin cause irregular periods?
Yes, high insulin levels can cause irregular periods. This is because insulin is a hormone that helps to regulate the menstrual cycle. When insulin levels are too high, it can disrupt the normal balance of hormones, which can lead to irregular periods.
How does Insulin Resistance change during each phase of the menstrual cycle?
What triggers insulin resistance?
There's no single cause of insulin resistance. Instead, it's a combination of certain genetic and lifestyle factors that can lead to the condition. These include:
- Genetics: If you have a family member with type 2 diabetes, you're more likely to develop the condition yourself.
- Obesity: Excess weight, especially around the waist, is a trigger for insulin resistance.
- Inactivity: A sedentary lifestyle can contribute to the development of insulin resistance.
- Age: The risk for insulin resistance increases as you get older.
- Ethnicity: Insulin resistance is more common in certain ethnic groups, such as Native Americans, African Americans, Hispanics, and Asians.
These are the general factors that can trigger insulin resistance, In the next section we shall talk more about how the menstrual cycle has a hand in insulin resistance.
Does ovulation cause insulin resistance?
There is some evidence that ovulation may cause insulin resistance. One study found that women who ovulated had higher levels of insulin and C-peptide (a marker for insulin resistance) than women who did not ovulate.
Moreover, the study “Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis” found that women with Polycystic Ovarian Syndrome (PCOS), are often associated with insulin resistance and defects in insulin secretion, which explains the increased prevalence of glucose intolerance in PCOS.
These studies suggest that there may be a link between ovulation and insulin resistance, but more research is needed to confirm this. If you're concerned about your risk of insulin resistance, talk to your healthcare provider
Is insulin sensitive during the luteal phase?
As mentioned in a previous section, insulin sensitivity is higher in the follicular phase (pre-ovulation) and decreased in the luteal phase (post-ovulation).
Studies also show that, during the luteal phase, there would be an increase in circulating insulin and a reduction in circulating glucose and triglycerides.
What factors worsen insulin resistance?
A few major factors that can worsen insulin resistance are
- Obesity
- Smoking
- Drinking excessive amounts of alcohol
- Eating high amounts of processed foods,
- Refined carbohydrates
- Foods with added sugars
- Certain physical conditions like PCOS and hormone imbalance
- Certain medical conditions (i.e acanthosis nigricans skin disorder, high cholesterol, and high blood pressure).
- Lack of physical activity
- Certain medications (i.e. corticosteroids and some types of antidepressants)
What is the fastest way to cure insulin resistance?
While it is almost impossible to completely cure insulin resistance. However, you can help your body’s cells become more receptive to insulin by
- Exercise: all types of exercise can support reversing insulin resistance, however greater exercise volumes and higher exercise intensities, including high-intensity interval training (HIIT) or sprint interval training (SIT) has been shown to be the most effective
- Nutrition: eating foods that have a low to medium glycemic index and limiting foods that have a high glycemic index
How does the menstrual cycle affect diabetes?
Hormone changes, especially during your menstrual cycle, can affect a person's diabetes. Hormonal fluctuations and hormonal imbalances cause blood glucose and insulin fluctuations. So women with diabetes should take extra care in managing these changes.
What are the factors that influence glucose levels during menstruation?
Several factors can influence blood sugar levels during menstruation. One of the most significant factors is diet and nutrition.
Diet and Nutrition
Studies have shown that women who consume a diet high in carbohydrates and processed foods may experience greater blood sugar fluctuations during the menstrual cycle.
Exercise and Physical Activity
Recent studies suggest that regular physical activity (PA) can lower the risk of insulin resistance. Exercise with higher energy expenditure such as high-intensity interval training (HIIT), produces greater results. However, both aerobic and resistance exercises can improve glucose regulation.
You can read the study review here: Update on the effects of physical activity on insulin sensitivity in humans
Medications and Other Health Conditions
Other factors that may influence blood sugar levels during the menstrual cycle include medications and other health conditions.
Strategies for Managing Blood Sugar During the Menstrual Cycle
Managing blood sugar levels during the menstrual cycle can be challenging, but there are several strategies that women can use to help regulate their blood sugar levels. One of the most important strategies is to eat a healthy diet. Women should consume foods that are low in carbohydrates and high in fiber, such as whole grains, fruits, and vegetables.
Regular exercise can also help to regulate blood sugar levels during menstruation. Women should aim to get at least 150 minutes of moderate-intensity exercise per week. Other strategies for managing blood sugar levels during the menstrual cycle include managing stress, getting adequate sleep, and taking medications as prescribed.
Tracking your Blood Sugar During the Menstrual Cycle
Tracking blood sugar during the menstrual cycle can be done using a blood glucose meter or continuous glucose monitoring system (CGM).
These devices can provide real-time information on blood sugar levels and help identify patterns and fluctuations over time. It's also important to keep a menstrual cycle calendar or app to track the menstrual cycle phases and note any changes in blood sugar levels.
This information can help in adjusting diet, exercise, and medication to manage blood sugar levels during the menstrual cycle. It's important to consult with a healthcare provider for guidance on tracking and managing blood sugar levels during the menstrual cycle.
Lifestyle Changes to Improve Blood Sugar Control
Here are a few simple, lifestyle changes that can help improve your blood sugar levels.
Lifestyle changes:
- Drink less sugar (avoid juices and sugary drinks)
- Avoid crash diets
- Don’t skip meals
- Build new healthy food habits slowly and consistently
- Mix and match different healthy food options
Diet guidelines:
- Include vegetables: dark green, leafy veggies like spinach
- Do not overconsume carbs like potatoes, peas, and corn
- Add plenty of fruits
- Add high-fiber food items: Almonds, black beans, broccoli, lentils, and oatmeal
- Avoid processed food: white bread and pasta
- Add lean protein: chicken, fish, egg whites, beans, lentils, and nut butter
- Include healthy fats: olive, sunflower, and sesame oils
- Check out our article on how to eat healthy when eating out
Conclusion
In summary, the menstrual cycle can have a significant impact on blood sugar levels in women, particularly during the luteal phase of the cycle.
Women with diabetes should monitor their blood sugar levels regularly and take steps to manage their blood sugar levels. By understanding the relationship between the menstrual cycle and glucose levels and adopting healthy lifestyle habits, women can improve their overall health and well-being.
References:
- American Diabetes Association. (2019). Menstruation and Diabetes.
- Fadl, H., Magnuson, A., Östlund, I., Montgomery, S., & Hanson, U. (2011). The impact of menstrual cycle on glucose control and risk of hypoglycaemia in type 1 diabetes mellitus. Diabetologia, 54(9), 2333-2338. doi: 10.1007/s00125-011-2213-3
- Garg, S. K., Hirsch, I. B., Skyler, J. S., & Cryer, P. E. (2017). Diabetes and Menstruation. Diabetes Care, 40(9), 1116-1119. doi: 10.2337/dc17-0931
- Hamilton, E. J., & Rakic, V. (2019). Menstrual Cycle-Dependent Variability in Blood Glucose Responses to Carbohydrate Consumption in Healthy Women. Nutrients, 11(12), 2925. doi: 10.3390/nu11122925
- Reeves, G. V., Fiske, D. N., & Friedman, M. I. (2017). Blood Glucose Response to Continuous, High-Intensity Interval Exercise and Moderate-Intensity Exercise During the Follicular and Luteal Phases of the Menstrual Cycle. International Journal of Exercise Science, 10(4), 570-579.
- NCIB (2010) - Insulin resistance/hyperinsulinemia and reproductive disorders in infertile women
- PubMed (1997) - Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis
- NCIB (2013) - Blood glucose levels, insulin concentrations, and insulin resistance in healthy women and women with premenstrual syndrome: a comparative study
- Madsen SM, Thorup AC, Overgaard K, Jeppesen PB. High Intensity Interval Training Improves Glycaemic Control and Pancreatic β Cell Function of Type 2 Diabetes Patients.
- Lin, G., Siddiqui, R., Lin, Z., Blodgett, J. M., Patel, S. N., Truong, K. N., & Mariakakis, A. (2023). Blood glucose variance measured by continuous glucose monitors across the menstrual cycle. Npj Digital Medicine, 6(1), 1-8. https://doi.org/10.1038/s41746-023-00884-x



